Acanthocytosis (Spur Cell Anemia): Causes, Symptoms, Diagnosis & Treatment Guide
Acanthocytosis (Spur Cell Anemia): Causes, Symptoms, Diagnosis & Treatment Guide
Learn about Acanthocytosis and spur cells, including causes like abetalipoproteinemia, neuroacanthocytosis, and liver disease. Understand symptoms, risk factors, diagnosis, complications, and treatment options.
What Is Acanthocytosis?
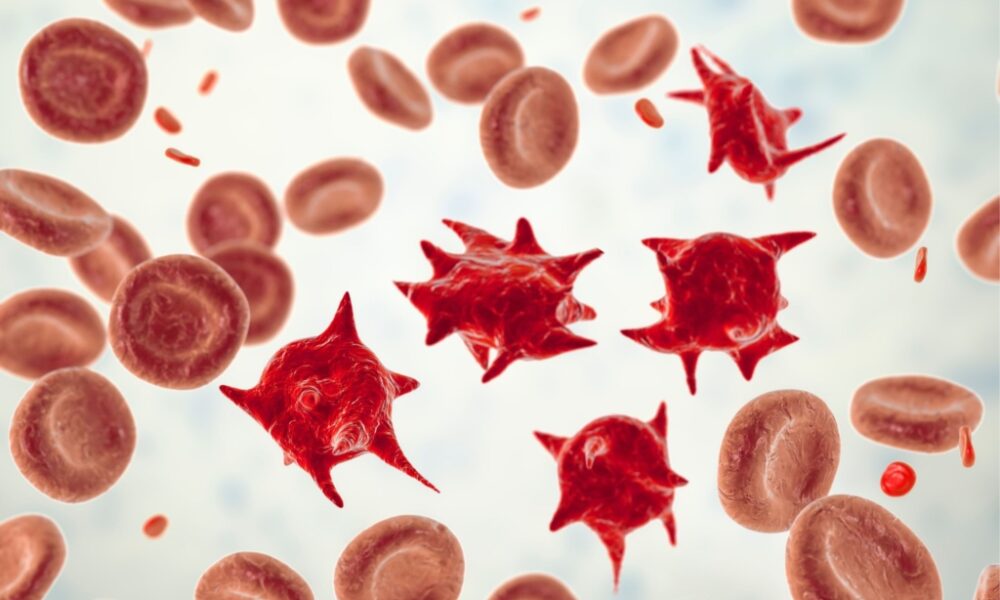
Acanthocytosis refers to the presence of acanthocytes (spur cells) in the bloodstream.
Acanthocytes are abnormally shaped red blood cells with irregular, spiky projections on their surface.
These cells appear rigid, contracted, and uneven, which makes them more likely to be destroyed in the spleen, leading to hemolytic anemia.
The main cause of acanthocyte formation is altered lipid composition of the red blood cell membrane, which affects its shape and flexibility.
Acanthocytes vs Echinocytes (Spur Cells vs Burr Cells)
| Feature | Acanthocytes (Spur Cells) | Echinocytes (Burr Cells) |
| Shape | Few irregular, uneven spikes | Many small uniform projections |
| Cause | Genetic/metabolic disorders, severe liver disease | Dehydration, artifact, kidney disease, enzyme defects |
| Clinical Impact | Significant — often pathological | Sometimes artifact-related, may be reversible |
Who Can Develop Acanthocytosis?
- Most commonly seen in infancy or childhood (in genetic disorders)
- Occurs in both sexes equally
- Found across all ethnic groups
- May appear later in life in cases related to liver disease or malnutrition
Genetic Background (Updated Understanding)
One major hereditary form is Chorea-Acanthocytosis, caused by mutations in the VPS13A gene.
- The VPS13A gene produces a protein called chorein, whose function likely involves cell membrane lipid transport.
- Mutations result in abnormal red blood cells and progressive neurological symptoms.
Inheritance Pattern
This condition follows an autosomal recessive inheritance pattern.
Carriers typically show no symptoms, but when both parents carry the mutation, their child has a 25% chance of being affected.
Common Conditions Associated with Acanthocytosis
| Condition | Key Features |
| Abetalipoproteinemia (Bassen-Kornzweig Syndrome) | Fat malabsorption, vitamin E deficiency, neurological decline |
| Severe Liver Disease (Spur Cell Anemia) | Advanced cirrhosis, rapid hemolysis |
| Neuroacanthocytosis Syndromes | Movement disorders, behavioral changes, seizures |
| Hypothyroidism | Can cause reversible acanthocytosis |
| Severe Malnutrition / Anorexia Nervosa | Vitamin E deficiency affects RBC membrane stability |
| McLeod Syndrome | Neurologic + cardiac abnormalities |
Signs and Symptoms
Symptoms depend on the underlying cause.
Blood-Related Signs
- Fatigue and weakness
- Pale skin (pallor)
- Jaundice
- Enlarged spleen (splenomegaly)
Eye Symptoms
- Progressive night blindness
- Loss of visual clarity and color vision
- Nystagmus (involuntary eye movements)
Digestive Symptoms
- Chronic diarrhea or bulky stools
- Abdominal swelling
- Liver enlargement (hepatomegaly)
Neurological Symptoms (Especially in Neuroacanthocytosis)
- Loss of reflexes
- Muscle stiffness or weakness
- Involuntary body movements (chorea)
- Gait difficulty or inability to walk
Diagnosis
Medical Tests Used
| Test | Purpose |
| Peripheral Blood Smear | Detects acanthocytes |
| Lipid Profile | Low cholesterol, LDL, VLDL in abetalipoproteinemia |
| Liver Function Tests | Identifies liver disease |
| Vitamin Level Tests | Low fat-soluble vitamins A, D, E, K |
| Genetic Testing | Confirms VPS13A or MTP mutations |
| Nerve Conduction Study | Detects neuropathy |
Complications
- Severe hemolytic anemia
- Progressive loss of vision
- Muscle wasting and movement disability
- Heart rhythm problems (in McLeod syndrome)
- Permanent nerve damage if untreated
Treatment (Based on Cause)
There is no universal cure — treatment targets the underlying disease.
Common Management Approaches
- High-dose Vitamin E supplementation (to protect nerves and RBC membranes)
- Medium-chain triglyceride (MCT) diet in abetalipoproteinemia
- Iron and folate supplements
- Thyroid hormone replacement in hypothyroidism
- Nutritional rehabilitation in malnutrition or anorexia
- Liver disease treatment and monitoring
- Physical and occupational therapy for neurological symptoms
- Splenectomy (removal of spleen) in severe hemolysis (rare and last-resort)
Prevention and Genetic Counseling
- Genetic counseling is recommended for families with inherited forms.
- Early diagnosis prevents progression of nerve and vision damage.
- Prenatal genetic testing can identify risk in pregnancy.
FAQs
Q 1. Is Acanthocytosis reversible?
Some forms (like those caused by malnutrition or hypothyroidism) can improve after treatment.
Genetic forms are not reversible, but symptoms can be managed.
Q 2. Can a healthy person develop acanthocytes temporarily?
Yes — dehydration and stored blood samples can form echinocytes that resemble acanthocytes, but they are not the same.
Q 3. Is Acanthocytosis life-threatening?
It can be, especially in cases of severe liver disease or untreated neurological forms.
For Detailed Guides and Health Articles Visit: https://healthcaretipshub.com/






