What Is Humira®?(adalimumab)
What is Humira?
Humira (adalimumab) is a tumor necrosis factor (TNF) blocker that reduces the effects of a substance in the body that can cause inflammation.
Humira is used to reduce the signs and symptoms of moderately to severely active rheumatoid arthritis (RA), polyarticular juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, plaque psoriasis, and and a chronic skin condition called hidradenitis suppurativa. It is also used reduce the signs and symptoms of moderately to severely active Crohn’s disease or moderately to severely active ulcerative colitis, after other drugs have been tried without successful treatment of symptoms.
Humira is also used to treat non-infectious intermediate, posterior and panuveitis in adult patients.
HUMIRA (adalimumab) is a recombinant human IgG1 monoclonal antibody specific for human tumor necrosis factor (TNF). HUMIRA was created using phage display technology resulting in an antibody with human derived heavy and light chain variable regions and human IgG1:k constant regions. Adalimumab is produced by recombinant DNA technology in a mammalian cell expression system and is purified by a process that includes specific viral inactivation and removal steps. It consists of 1330 amino acids and has a molecular weight of approximately 148 kilodaltons.
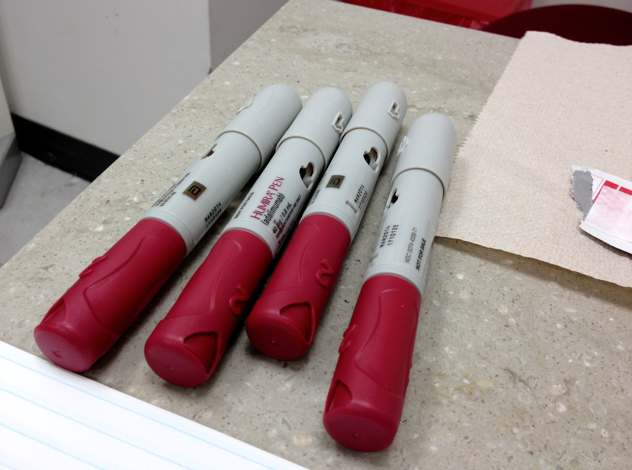
HUMIRA is supplied as a sterile, preservative-free solution of adalimumab for subcutaneous administration. The drug product is supplied as either a single-use, prefilled pen (HUMIRA Pen), as a single-use, 1 mL prefilled glass syringe, or as a single-use institutional use vial. Enclosed within the pen is a single-use, 1 mL prefilled glass syringe. The solution of HUMIRA is clear and colorless, with a pH of about 5.2.
Each 80 mg/0.8 mL prefilled syringe delivers 0.8 mL (80 mg) of drug product. Each 0.8 mL of HUMIRA contains adalimumab 80 mg, mannitol 33.6 mg, polysorbate 80 0.8 mg, and Water for Injection, USP.
Each 40 mg/0.4 mL prefilled syringe or prefilled pen delivers 0.4 mL (40 mg) of drug product. Each 0.4 mL of HUMIRA contains adalimumab 40 mg, mannitol 16.8 mg, polysorbate 80 0.4 mg, and Water for Injection, USP.
Each 40 mg/0.8 mL prefilled syringe, prefilled pen, or single-use institutional use vial delivers 0.8 mL (40 mg) of drug product. Each 0.8 mL of HUMIRA contains adalimumab 40 mg, citric acid monohydrate 1.04 mg, dibasic sodium phosphate dihydrate 1.22 mg, mannitol 9.6 mg, monobasic sodium phosphate dihydrate 0.69 mg, polysorbate 80 0.8 mg, sodium chloride 4.93 mg, sodium citrate 0.24 mg and Water for Injection, USP. Sodium hydroxide is added as necessary to adjust pH.
Each 20 mg/0.4 mL prefilled syringe delivers 0.4 mL (20 mg) of drug product. Each 0.4 mL of HUMIRA contains adalimumab 20 mg, citric acid monohydrate 0.52 mg, dibasic sodium phosphate dihydrate 0.61 mg, mannitol 4.8 mg, monobasic sodium phosphate dihydrate 0.34 mg, polysorbate 80 0.4 mg, sodium chloride 2.47 mg, sodium citrate 0.12 mg and Water for Injection, USP. Sodium hydroxide is added as necessary to adjust pH.
Each 10 mg/0.2 mL prefilled syringe delivers 0.2 mL (10 mg) of drug product. Each 0.2 mL of HUMIRA contains adalimumab 10 mg, citric acid monohydrate 0.26 mg, dibasic sodium phosphate dihydrate 0.31 mg, mannitol 2.4 mg, monobasic sodium phosphate dihydrate 0.17 mg, polysorbate 80 0.2 mg, sodium chloride 1.23 mg, sodium citrate 0.06 mg and Water for Injection, USP. Sodium hydroxide is added as necessary to adjust pH.
Important information
Some people using Humira have developed a rare fast-growing type of lymphoma (cancer). This condition affects the liver, spleen, and bone marrow, and it can be fatal. Humira can also lower blood cells that help your body fight infections and help your blood to clot. Serious and sometimes fatal infections may occur during treatment with Humira.
Call your doctor at once if you have symptoms such as fever, night sweats, weight loss, feeling full after eating only a small amount, pain in your upper stomach, easy bruising or bleeding, dark urine, or jaundice (yellowing of the skin or eyes).
Humira can lower blood cells that help your body fight infections and help your blood to clot. Your blood may need to be tested often. Avoid being near people who are sick or have infections. Avoid activities that may increase your risk of bleeding injury. Serious and sometimes fatal infections may occur during treatment with Humira. Tell your doctor at once if you develop signs of infection.
How Humira affects autoimmune diseases
Humira can bring relief from symptoms of autoimmune diseases such as rheumatoid arthritis.
An autoimmune disease is one in which the body’s immune system falsely detects and attacks a threat within the body that does not really exist.
This can lead to a number of problems and conditions, including rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, and psoriasis.
Experts are unsure exactly what causes autoimmune diseases, but tumor necrosis factor alpha (TNFα) appears to be a major contributor to inflammation in these diseases.
TNFα triggers inflammation when the body is under threat, and the immune system goes into action to protect it. However, too much TNFα can attack healthy tissue and cause inflammation.
Humira binds to TNFα and blocks its inflammatory effect. This reduces pain and inflammation in patients with autoimmune diseases.
The word HUMIRA stands for HUman Monoclonal Antibody In Rheumatoid Arthritis.
How to use Humira
Humira is a long-term treatment. Patients respond at different speeds to its analgesic and anti-inflammatory effects. According to the manufacturers, Abbvie, some people see benefits after 2 weeks, while others may need to take it for 3 months or longer to seen an improvement.
It is vital for the patient to adhere to the treatment plan for best results. Those who stop taking their medications are most likely to have overactive immune systems again.
How to use the Humira pen or syringe
Humira is injected into either the abdomen or the thighs, using a prefilled pen or syringe. The injection should not be given in skin that is bruised or tender, or where there are patches of psoriasis.
Patients normally administer Humira themselves. A single-use pen contains 40 milligrams of medication, while a syringe may contain 40, 20, or 10 milligrams.
Humira use begins with a starting dose, followed by regular doses, normally every second week. A doctor will advise the patient about their dosage requirements.
There are specific instructions for storage and use, and patients are advised not to use the Humira pen or syringe without first being shown by a doctor and without reading the full instructions.
Patients are advised to practice first with a health care professional, to ensure they are not startled by the click when administering the dose.
Use Humira exactly as prescribed by your doctor. Follow the directions on your prescription label. Do not use this medicine in larger or smaller amounts or for longer than recommended. Use Humira regularly to get the most benefit. Get your prescription refilled before you run out of medicine completely.
The dose schedule for Humira is highly variable and depends on the condition you are treating. You may need an injection only every other week. Or you may need up to 4 injections in 1 day for 2 days in a row. Follow your doctor’s dosing instructions very carefully.
Do not start using Humira if you have any signs of an infection (fever, chills, night sweats, weight loss, body aches, tiredness, cough with mucus, feeling short of breath, skin sores, stomach pain, diarrhea, pain or burning when you urinate). Call your doctor for instructions.
Humira is injected under the skin. You may be shown how to use injections at home. Do not self inject this medicine if you do not fully understand how to use the injection and properly dispose of used needles and syringes. Do not inject Humira into skin that is bruised, red, tender, or hard.
Each prefilled syringe is for one use only. Throw away after one use, even if there is still medicine left in it after injecting your dose. Do not use a prefilled syringe if it looks cloudy or has particles in it. Call your pharmacist for new medicine.
Use a disposable needle and syringe only once. Follow any state or local laws about throwing away used needles and syringes. Use a puncture-proof “sharps” disposal container (ask your pharmacist where to get one and how to throw it away). Keep this container out of the reach of children and pets.
Adalimumab can lower blood cells that help your body fight infections and help your blood to clot. This can make it easier for you to bleed from an injury or get sick from being around others who are ill. Your blood may need to be tested often. Serious and sometimes fatal infections may occur during treatment with Humira. Contact your doctor right away if you have signs of infection such as: fever, chills, sore throat, or flu symptoms.
If you need surgery, tell the surgeon ahead of time that you are using Humira.
If you have ever had hepatitis B, Humira can cause this condition to come back or get worse. You will need frequent blood tests to check your liver function during treatment and for several months after you stop using this medicine.
Store in a refrigerator. If you travel with a prefilled syringe, keep it in a small cooler with an ice pack and protect it from light. Do not remove the prefilled syringe from the refrigerator or cooler until you are ready to give yourself an injection.
Do not freeze, and throw away the medicine if it has become frozen.
HUMIRA is a prescription medicine used:
- To reduce the signs and symptoms of:
- Moderate to severe rheumatoid arthritis (RA) in adults. HUMIRA can be used alone, with methotrexate, or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Moderate to severe polyarticular juvenile idiopathic arthritis (JIA) in children 2 years of age and older. HUMIRA can be used alone, with methotrexate, or with certain other medicines.
- Psoriatic arthritis (PsA) in adults. HUMIRA can be used alone or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Ankylosing spondylitis (AS) in adults.
- Moderate to severe Crohn’s disease (CD) and to achieve and maintain clinical remission in adults who have not responded well to certain other medications. HUMIRA is also used to reduce signs and symptoms and to achieve clinical remission in these adults who have lost response to or are unable to tolerate infliximab.
- Moderate to severe Crohn’s disease (CD) and to achieve and maintain clinical remission in children 6 years of age and older when certain other treatments have not worked well enough.
- Moderate to severe hidradenitis suppurativa (HS) in adults.
- In adults, to help get moderate to severe ulcerative colitis (UC) under control (induce remission) and keep it under control (sustain remission) when certain other medicines have not worked well enough. It is not known if HUMIRA is effective in people who stopped responding to or could not tolerate anti-TNF medicines.
- To treat moderate to severe chronic plaque psoriasis (Ps) in adults who are ready for systemic therapy or phototherapy, and are under the care of a doctor who will decide if other systemic therapies are less appropriate.
- To treat non-infectious intermediate (middle part of the eye), posterior (back of the eye) and panuveitis (all parts of the eye) (UV) in adults.
Humira Side Effects
As Humira is an immunosuppressant, it will leave the body more prone to infections. The use of TNF blockers has also been linked to cancer, including some rare and unusual types of cancer.
Common adverse effects include, but are not limited to:
- Redness, rash, swelling, itching or bruising at the injection site
- Infections, especially upper respiratory infections and sinus infections
- Headaches and nausea
Some serious side effects require immediate medical attention.
Serious infections can occur due to the immunosuppressant qualities of Humira. These include tuberculosis (TB) and other infections caused by viruses, fungi, or bacteria.
Infections may develop in carriers of hepatitis B. Symptoms include fever and chills, muscle pain, fatigue, dark urine and a yellow tinge to the eyes of skin, loss of appetite, vomiting, clay-colored feces, stomach problems, and skin rash.
Some people may have an allergic reaction. Symptoms include chest tightness, wheezing, and other breathing difficulties, hives, itching, and skin rash, swelling of the tongue, lips, face and other parts of the body.
Nervous system problems may occur, leading to weakness in the arms and legs, numbness, tingling, visual disturbances and dizziness.
Blood problems may occur. A low platelet count can lead to an increased likelihood of bleeding, and a low level of white blood cells make it harder to fight infection. The patient may have a fever that does not go away, or finds they are bruising or bleeding easily.
Heart conditions can develop or get worse, leading to shortness of breath, sudden weight gain, and swelling in the hands and feet.
Immune reactions may occur. One example is a lupus-like syndrome, with chest pain and shortness of breath, joint pain, or a rash on the cheeks or arms that worsens when exposed to the sun.
Liver problems can arise, leading to fatigue, yellowish skin or eyes, vomiting and not wanting to eat, and abdominal pain.
Psoriasis may emerge or worsen.
Along with its needed effects, adalimumab (the active ingredient contained in Humira) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking adalimumab:
More common
- Abdominal or stomach fullness
- body aches or pain
- cough or hoarseness
- ear congestion
- gas with abdominal or stomach pain
- lightheadedness
- loss of voice
- lower back or side pain
- muscle aches and pains
- nasal congestion
- pain or tenderness around the eyes or cheekbones
- rapid and sometimes shallow breathing
- shivering
- sunken eyes
- thirst
- trouble sleeping
- warmth on the skin
- wrinkled skin
Less common
- Abdominal or stomach pain
- abnormal vaginal bleeding or discharge
- agitation
- arm, back, or jaw pain
- black, tarry stools
- bleeding from the gums or nose
- blindness
- bloating or swelling of the face, arms, hands, lower legs, or feet
- blood in the stool or change in bowel habits
- bloody or cloudy urine
- blurred vision
- broken bones
- change in size, shape, or color of an existing mole
- change in skin color
- chest pain
- chest tightness or heaviness
- chills
- clear or bloody discharge from the nipple
- cold hands and feet
- confusion
- constipation
- cough
- coughing or spitting up blood
- decreased urination
- decreased vision
- depression
- difficult or frequent urination
- difficulty with breathing
- difficulty, burning, or painful urination
- dimpling of the breast skin
- dizziness
- drowsiness
- eye pain
- fainting
- fast, slow, or irregular heartbeat
- fever
- forgetfulness
- frequent urge to urinate
- general feeling of illness
- hair loss
- hallucinations
- headache
- increased thirst
- inverted nipple
- irregular breathing
- irregular pulse
- irritability
- itching or rash
- light colored stools
- loss of appetite
- lump in the breast or under your arm
- lump or swelling in the abdomen or stomach
- mole that leaks fluid or bleeds
- muscle cramps or spasms
- nausea
- new mole
- night sweats
- no blood pressure or pulse
- noisy breathing
- numbness or tingling in your arms, legs, or face
- pain, redness, or swelling in the arms or legs without any injury present
- pale skin
- persistent non-healing sore on your skin
- pink growth
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- raised, firm, or bright red patch
- redness or swelling of the breast
- seizures
- sharp back pain just below your ribs
- shiny bump on your skin
- slurred speech or problems with swallowing
- sneezing
- sore on the skin of the breast that does not heal
- sore throat
- sores, ulcers, or white spots on the lips or mouth
- spitting up blood
- stiff neck
- stopping of the heart
- sudden high fever or low grade fever for months
- sweating
- swelling of the face, fingers, feet, or lower legs
- swollen glands
- swollen neck veins
- tightness in the chest
- tiredness
- trouble breathing with activity
- trouble thinking
- unconsciousness
- unexplained bruising or bleeding
- unpleasant breath odor
- unusual tiredness or weakness
- unusual weight gain or loss
- visual disturbances
- vomiting
- vomiting of blood or material that looks like coffee grounds
- yellow skin or eyes
Incidence not known
- Blistering, peeling, or loosening of the skin
- diarrhea
- joint or muscle pain
- pinpoint red spots on the skin
- red skin lesions, often with a purple center
- red, irritated eyes
- red, scaling, or crusted skin
- unusual bleeding or bruising
Infections
Patients treated with Humira are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids. Discontinue Humira if a patient develops a serious infection or sepsis.
Reported infections include:
- Active tuberculosis (TB), including reactivation of latent TB. Patients with TB have frequently presented with disseminated or extrapulmonary disease. Test patients for latent TB before Humira use and during therapy. Initiate treatment for latent TB prior to Humira use.
- Invasive fungal infections, including histoplasmosis, coccidioidomycosis, candidiasis, aspergillosis, blastomycosis, and pneumocystosis. Patients with histoplasmosis or other invasive fungal infections may present with disseminated, rather than localized, disease. Antigen and antibody testing for histoplasmosis may be negative in some patients with active infection. Consider empiric anti-fungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness.
- Bacterial, viral and other infections due to opportunistic pathogens, including Legionella and Listeria.
Carefully consider the risks and benefits of treatment with Humira prior to initiating therapy in patients with chronic or recurrent infection.
Monitor patients closely for the development of signs and symptoms of infection during and after treatment with Humira, including the possible development of TB in patients who tested negative for latent TB infection prior to initiating therapy.
Precautions
Patients should not take Humira if they are allergic to any medication containing adalimumab or Mannitol, sodium citrate, monobasic sodium phosphate dehydrate, sodium chloride, citric acid monohydrate, or polysorbate 80.
It is important to disclose any current medications and medical conditions before using Humira.
Humira should not be used by anyone with a severe infection, active TB, and other infections that may occur when the immune system is weakened.
It should not be taken with a number of drugs, including Kineret (anakinra) and Orencia (abatacept).
Before using Humira, the patient should ensure their doctor knows if they have or have ever had any of the medical conditions listed below:
- Any type of infection, including a localized one, such as a leg ulcer
- A fungal infection
- Allergy to latex or rubber
- Any heart condition
- Any type of autoimmune disease
- Any type of demyelinating disease, including multiple sclerosis
- Cancer
- Liver or kidney problems
- Recurrent infections, or any conditions which increase infection risk
The doctor also needs to know if the patient is taking any immunosuppressant medications, if they or anyone close to them has, or has had, tuberculosis (TB), and if the person is a carrier of the hepatitis B virus.
Some people may be able to get help with Humira from their insurance company. This link can provide more information.
Other products that work in a similar way, known as biosimilars, are also available. In September 2016, Amjevita gained the approval of the United States Food and Drug Administration (FDA).
Amjevita can also be used in cases of moderately to severely active polyarticular juvenile idiopathic arthritis from the age of 4 years.
For more information visit us our website: https://healthcaretipshub.com