Accessory Atrioventricular Pathways: Causes, Diagnosis, and Modern Ablation Treatments
Accessory Atrioventricular Pathways: Causes, Diagnosis, and Modern Ablation Treatments
Understanding Accessory Atrioventricular Pathways and Preexcitation Arrhythmias
Introduction
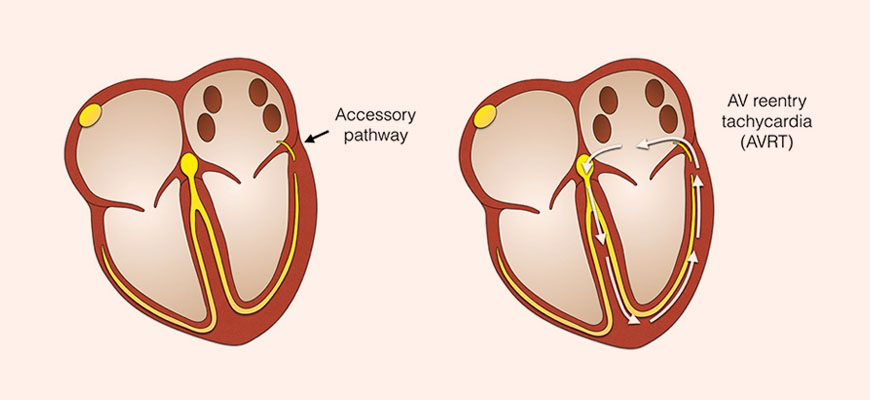
Accessory atrioventricular (AV) pathways are abnormal muscular connections that allow electrical impulses to travel directly between the atria and ventricles, bypassing the normal AV node-His-Purkinje conduction system. This results in ventricular preexcitation, often seen in Wolff-Parkinson-White (WPW) syndrome, and can lead to episodes of supraventricular tachycardia (SVT) and, in rare cases, life-threatening arrhythmias.
Embryological Basis
During early cardiac development, a ring of muscular tissue surrounds the atrioventricular canal. Normally, this tissue regresses, leaving only the AV node as the conduction bridge. However, if segments of this tissue persist, accessory pathways remain, forming abnormal atrioventricular conduction channels.
Clinical Presentation
Patients may present with:
- Palpitations and rapid heartbeats
- Syncope or dizziness
- Chest discomfort
- Preexcitation patterns on ECG (short PR interval + delta wave)
Some accessory pathways become clinically significant only during atrial fibrillation, where rapid conduction can trigger ventricular tachycardia or cardiac arrest.
Types and Locations of Accessory Pathways
Accessory pathways can be categorized based on their anatomical insertion:
| Location | Description | Clinical Note |
| Left Free Wall | Most common | Usually accessible via transseptal or retrograde aortic approach |
| Right Free Wall | Less common | Mapping may be more complex |
| Posteroseptal | Near coronary sinus | May require coronary venous or epicardial access |
| Anteroseptal | Near His bundle | High risk of AV block during ablation |
Diagnosis
Diagnosis includes:
- 12-lead ECG to identify preexcitation patterns
- Electrophysiology Study (EPS) to locate the pathway
- Holter monitoring for intermittent SVT
- Cardiac imaging if structural abnormalities are suspected
Treatment: Radiofrequency Catheter Ablation
Radiofrequency current is delivered through an ablation catheter to eliminate the accessory pathway. It has largely replaced surgical approaches due to:
- High success rate (≈ 95–99%)
- Low recurrence rate (≈ 5–10%)
- Reduced morbidity
Ablation may be performed:
- Endocardially via femoral or subclavian venous access
- Epicardially using a subxiphoid percutaneous approach when pathways are deep or inaccessible
- Via Coronary Sinus Tributaries for posteroseptal pathways
Epicardial Ablation Insights
Epicardial mapping is considered when:
- Multiple previous ablations have failed
- The pathway is located adjacent to coronary sinus musculature or diverticula
- Standard endocardial access is not feasible
In clinical studies:
- Success Rate: ~30% as standalone treatment
- Epicardial mapping helps guide repeat endocardial ablation in additional cases
Major complications are rare, but may include:
- Pericarditis
- Coronary sinus injury
- Tamponade (very rare with experienced operators)
Post-Ablation Care
- Observation for arrhythmia recurrence for 24–48 hours
- Anticoagulation if ablated near left-sided structures
- Repeat electrophysiology testing at 2–3 months if symptoms recur
Conclusion
Accessory atrioventricular pathways are a well-recognized cause of preexcitation arrhythmias such as WPW syndrome. Radiofrequency catheter ablation remains the gold-standard treatment with high cure rates and minimal complications. In difficult cases, epicardial or coronary venous approaches provide effective alternatives.
Early diagnosis and tailored ablation strategy are key to preventing long-term arrhythmia complications.
For Detailed Guides and Health Articles Visit: https://healthcaretipshub.com/






